A gait laboratory is a specialised facility equipped with technology that assesses human movement and gait pattern (the way a person walks).
This purpose-built lab includes a set of cameras, force plates and other measurement devices that capture and analyse the movement of various parts of the body during walking. This technology allows us to carry out a gait analysis which is a comprehensive evaluation of the way an individual stands and walks. This analysis can help identify the source of any muscle, nerve or skeletal problems that affect a person’s mobility.
Also known as a video vector gait laboratory or motion analysis laboratory, the gait lab provides precise and detailed measurements of joint angles, muscle activity and ground reaction forces. All of which are important for understanding and improving gait patterns with orthotics.
We use gait labs in a clinical setting to address and treat individuals with a range of movement disorders caused by neurological conditions including:
Individuals recovering from brain injury or stroke can also benefit from a gait lab assessment. As well as children who have undergone Selective Dorsal Rhizotomy (SDR) surgery.
At the London Orthotic Consultancy, we have state-of-the-art gait labs in three of our clinics. In Kingston-Upon-Thames, Cambridge and in Manchester, which utilises Salford Univeristy’s Gait Laboratory.

Gait analysis assessment at the London Orthotic Consultancy.
In 2023, we installed a brand new Contemplas Markerless Tracking Gaitlab with AMTI force plates and two new high-speed cameras in our Kingston clinic.
This state-of-the-art equipment offers highly accurate 3D kinematic data and operates at a higher frequency than previous models. This allows us to assess faster-moving gait patterns. The vectors projected into the video make use of this 3D data, giving our clinicians more data to utilise.
The markerless tracking technology also allows us to compare pre and post-gait patterns more effectively. This can help us objectively demonstrate improvements over time.
The Gait lab is fundamental to our OSKAR clinic work (Optimal Segmental Kinematic Alignment approach to Rehabilitation (OSKAR) with world-renowned physiotherapist Elaine Owen.
We use the gait lab to help us prescribe a range of orthoses. Most commonly for Ankle Foot Orthoses (AFOs), Knee Ankle Foot Orthoses (KAFOs) and carbon fibre orthoses.
In this video, LOC Director Sam Walmsley demonstrates how we use a gait lab analysis during a clinical orthotic assessment. Here we are using the gait lab to assess, prescribe and fine-tune a neuro swing orthosis for patient Quentin.
A video vector gait laboratory has several components:
Gait labs like ours measure force in three planes; sagittal, coronal and transverse. The technology creates a vector or graphical representation of this force which is then projected on to the camera footage of the person walking.
The result is that we can accurately see where the vector is located. In particular, its direction and where it is in relation to the joints in the stance leg. Understanding where the force is positioned in relation to the leg is essential for accurate fine-tuning of the lower limb orthotics that we prescribe.
For example, if the vector is positioned too far in front of the knee at late mid-stance, there will be a hyperextension force applied to the knee. The aim of our work within the gait laboratory will be to produce prescriptions that are designed to:
Gait analysis laboratories can significantly improve the assessment, production and fitting of orthotics in the following ways:
Getting real-time feedback during walking or other activities can help clinicians and orthotists evaluate the effectiveness of the orthotics prescribed and make adjustments as required immediately.
Incredibly precise measurements of joint angles, muscle activity and ground reaction forces means we can create orthotics that fit and function optimally.
Gait laboratory data is objective (unlike human bias) which can help in identifying specific areas of weakness or dysfunction and track progress over time.
No two patients are the same, so when it comes to orthotics, it’s not a case of one-size-fits-all. Gait lab data can help our orthotists create even more bespoke treatment plans for patients, based on their specific gait patterns and their individual goals.
Detailed information and feedback from gait laboratories mean better and more effective orthotics, leading to better outcomes for patients.
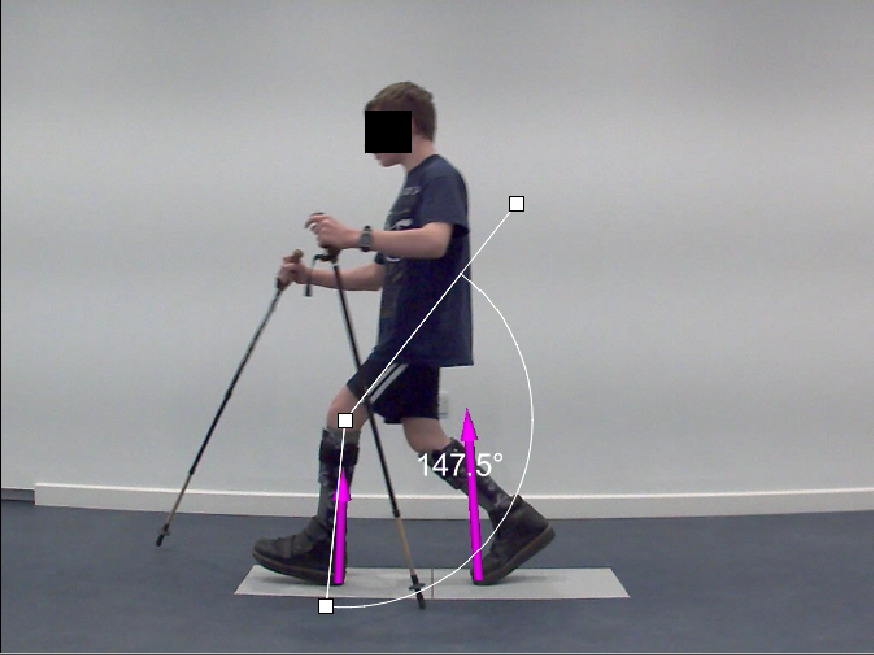
Gait analysis technology used during clinical paediatric orthotic assessment. The overlaid video vectors highlight the force measurements and angles created when walking.

Join The London Orthotic Consultancy in celebrating Cerebral Palsy Awareness Day on March 25th. Learn just how important expert orthotic care is in enhancing mobility, independence, and quality of life for children and adults with cerebral palsy.

Introducing the Agilik™ smart orthosis, a cutting-edge, powered knee orthotic now available in the UK through the London Orthotic Consultancy. Unlike traditional KAFOs or heavy exoskeletons, the Agilik™ provides dynamic knee assistance and offers real-time support, reducing fatigue and improving posture. This pioneering, modern technology can help children and adults with lower limb weakness walk more efficiently and naturally. We are honoured to be selected as the exclusive paediatric specialist centre in the UK for the Agilik™ device.

When Sophie noticed her baby Max had a persistent flat spot on his head, she was told it would resolve naturally—but it didn’t. Seeking a second opinion led her to the London Orthotic Consultancy, where Max was diagnosed with severe plagiocephaly.

A little more than four years after the LOCband Lite's launch, we're proud to have successfully treated our 250th helmet therapy patient at our Romford clinic using our cutting-edge 3D-printed cranial band. After five months of treatment, her final scan showed that her asymmetry had decreased from 12 mm to 3 mm.

Sky News published an article this month quoting scientists at Southmead Hospital who claimed there was a lack of research into flat head syndrome and its treatment with cranial remoulding (helmet) therapy. This is our response.

With our non-surgical treatment plan, Alex achieved 100% chest correction in just two years. His treatment involved a combination of dynamic chest compressor and vacuum bell therapy treatment to address his pectus excavatum and rib flaring.

Learn how a custom carbon fibre AFO helped Gill regain mobility and comfort despite complex challenges from shin bone (tibia) removal. We created a truly tailored orthotic solution made from pre-preg carbon fibre at our Cambridge clinic.

Discover how bespoke orthotics and the OSKAR program with Elaine Owen transformed Archie’s life with cerebral palsy quadriplegia, helping him avoid a wheelchair and achieve greater mobility.