Pectus excavatum is the most common form of congenital chest deformity, also referred to as ‘sunken’ or ‘funnel’ chest. Pectus excavatum occurs in an estimated 1 in 300-400 births (Medscape). It’s also 3-5 times more common in men.
It happens when the chest bone is pushed inwards by an overgrowth of cartilage between the ribs and the breast bone. The condition tends to become exaggerated during puberty where growth spurts cause the cartilage and bones to grow at a rapid rate. The sternum becomes caved in, looking “dented” or “sunken”. The ribs often tend to flare out as a result of the excavatum area sinking inwards. Scoliosis is also associated with the disorder.
After puberty, the bones and cartilage in the chest stop undergoing growth spurts and therefore the chest will remain ‘stable’ when a person reaches adulthood.
For patients considering LOC’s non-surgical treatment for pectus excavatum, we offer the opportunity for an initial free consultation via Skype, Facetime or Zoom. During this one of our specialist clinicians will give a detailed explanation of our treatment programme, discuss your individual symptoms and assess your suitability for treatment.
The cause of pectus excavatum is unknown, though the condition is thought to happen as a result of abnormal cartilage growth, between the bony ribs and the breastplate, causing the sternum – or breastbone – to buckle inwards (when it protrudes outwards, this is referred to as pectus carinatum).
There is thought to be a hereditary aspect as patients with pectus usually have family members that have gone through the same. According to the American Board of Family Medicine, about 40% of pectus patients have family members with pectus deformity but a genetic link is not yet fully understood.
Pectus excavatum is also associated with rare musculoskeletal syndromes like Marfan syndrome.
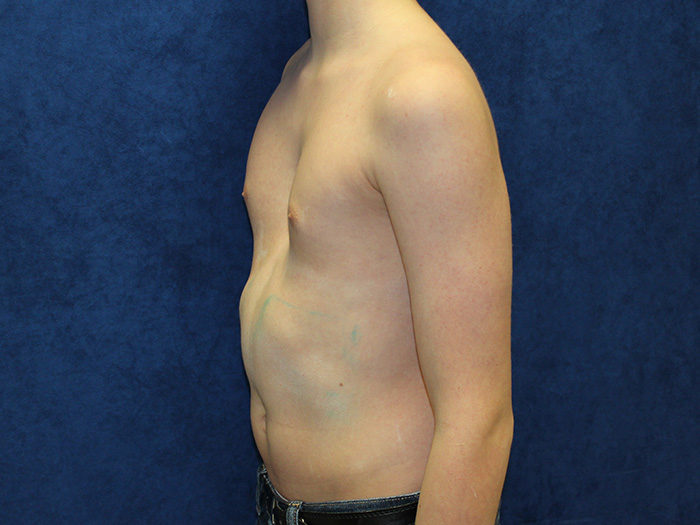
Those with pectus excavatum will characteristically have their breast bone – or sternum – appear ‘sunken’ into the chest, like a dent. The severity of the ‘sunken’ excavatum area can vary greatly from patient to patient, and some may also have asymmetrical cartilage growth. Ribs flaring out below the excavatum area is also a common feature.
Many who have pectus excavatum do not experience any further symptoms outside of their appearance. Some have other associated complications listed below.
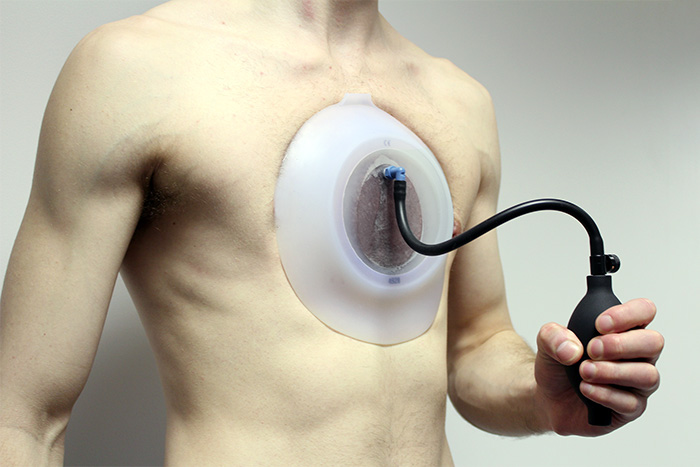
Pectus excavatum patient using the vacuum bell
Having pectus excavatum is made more difficult by the reduced self-esteem which often accompanies it. While some people accept the shape of their chest, for others it can be a daily source of anxiety, low self-confidence and increased self-consciousness. Some cases are more drastic than others, and adolescents may find the appearance of their chest disturbing or worry about others seeing it.
Issues with self-esteem and body image perception may become exacerbated during teenage years. In a 30 year Californian study carried out by UCLA School of Medicine the most common complaint from young patients was related to the unattractive physical appearance of the deformity. The psychological effects are normally enough to warrant the need to seek corrective help.
Sometimes other problems associated with pectus excavatum include:
Though not universal, we don’t want to overstate the potential respiratory or heart problems associated with the condition. Many people with a pectus deformity do not suffer from any of the above. Many patients find the psychological distress caused by having a pectus deformity much more distressing than its stated complications.
The London Orthotic Consultancy’s treatment programme for pectus excavatum involves wearing a bespoke brace – the Dynamic Chest Compressor – in combination with the use of a device called the 'Vacuum Bell' and a programme of Yoga exercises that have been developed specifically to augment our non-surgical treatment.
The dynamic chest compressor works on the flared ribs that are stereotypical of pectus deformity. Sometimes rib flaring can significantly contribute to the excavatum deformity and without addressing it, patients may find the overall result unsatisfactory.
The Vacuum Bell was invented by Eckart Klobe, a graduate in chemical engineering. The mechanism uses a suction cup to create a vacuum at the anterior chest wall and this lifts the sternum (breastbone) up and out. The brace is used in conjunction with the vacuum bell to correct rib flaring.
We have taken a holistic approach to the exercises that are an integral part of our treatment programme; they are Yoga exercises that have been developed specifically to augment our non-surgical treatment. The exercises encourage correct breathing and posture and general stretching of the chest area. Deep breathing exercises allow the lungs to expand against the chest wall, pushing it outwards.
Dr Haje pioneered the non-surgical treatment of pectus excavatum and demonstrated that it was possible to improve chest wall shape using his methods. He showed that the chest wall shape could be improved with a combination of bracing and exercise treatment.

We offer free online pectus excavatum and pectus carinatum consultations via Skype, Facetime or Zoom for those worried about their chest shape.
Our treatment programme will be explained in detail so you can see whether treatment is right for you.

LOC's non-surgical treatment for pectus involves the Dynamic Chest Compressor, a custom made orthosis designed for an individual’s anatomy to specifically treat their particular type of pectus. For Pectus Excavatum patients we also prescribe the Vacuum Bell - it works by using a silicone cup and a vacuum pump to create an area of low pressure over the sunken part of the chest.
We manufacture bespoke braces for each patient, ensuring comfort and ease of compliance during treatment.

The London Orthotic Consultancy has been providing non-surgical pectus treatment since 2010 achieving positive results in our patients.
We are proud to be the pioneers of this treatment in the UK and are happy to share some patient successes for those who have undergone Pectus Excavatum treatment with us.

LOC's pectus treatment is non-surgical and involves wearing a bespoke brace or orthosis called a 'Dynamic Chest Compressor', combined with a programme of Yoga exercises that have been developed specifically to augment our non-surgical treatment.
Most NHS trusts no longer recommend surgery for pectus carinatum and pectus carinatum as the conditions are considered to be cosmetic and no threat to physical health.
Our experience and development of custom-made braces has led to many patient success stories.

LOC director and pectus specialist, Sam Walmsley, has recorded a series of videos answering our client's frequently asked questions about our pectus treatments and exercise programmes.
For patients who want to avoid surgery, non-surgical pectus treatment can be a great way to achieve a flatter chest, but often, patients are unsure of what treatment involves.

We offer orthotic treatment for international patients seeking non-surgical pectus excavatum and pectus carinatum bracing in the UK. Our specialist clinicians have extensive experience treating pectus deformity patients from around the world.
We regularly treat international patients with our evidence-based orthotics including those from Europe, South America and the Middle East.
This depends on several factors; the position of the chest wall deformity, its severity, the flexibility of the chest, the kind of results wanting to be achieved and the age of the person undergoing treatment for pectus excavatum or pectus carinatum.
Early adolescence (roughly between the ages of 12-16 years old) – is an optimum age to start treatment, given that the chest is still maturing, and flexible, permanent correction is more easily achievable. Once bracing treatment is complete and a patient has stopped growing, the deformity will not return. For younger pectus patients, conservative bracing is used to keep a deformity from worsening and can help them to avoid surgery in later life.
For older pectus patients (between the ages of 20 to 30) results can be harder to achieve, as the costal cartilage hardens into the bone as a person matures. Over the years we have successfully treated many adults for both pectus excavatum and pectus carinatum and active adults with flexible chests can expect good results.
Again, this hugely depends on what a patient wants to achieve from treatment; whether that’s avoidance of surgery, improvement in the appearance of the chest shape, reduction in rib flaring etc. All these goals are taken into consideration during your first consultation. While there are no serious health risks of having pectus carinatum or excavatum – beyond the cosmetic – for many patients and parents, treatment outcomes involve improving confidence and self-esteem. During our 2018 Pectus Patient Survey, 92% of pectus carinatum patients surveyed said that treatment had a ‘major improvement’ or ‘an improvement’ on their social life.
You can read the results of our 2018 Pectus Patient Survey and quality of life questionnaire here.
Regular reviews are part of the treatment programme, preferably in clinic with one of our specialist orthotists, or via Skype consultations.
The number of appointments needed will vary from patient to patient but as a general rule, younger pectus patients who are growing at a faster rate will need to be seen more regularly for check-up appointments. This is to ensure that the brace fits well and is guiding the chest into the correct position as growth spurts occur. For other patients, this can be scaled back according to their individual needs and demands.
Regular appointments are beneficial for assessing progress, checking for signs of rubbing and determining whether another brace is needed. Appointments are also good for checking patient compliance to brace wearing and the breathing and exercise programme. At each appointment, we make time for patients to see our physiotherapist to fine-tune their exercise programme and check to see how a patient has been managing with the current programme.
We always advise coming in for appointments whenever you have any concerns about the brace or treatment programme, especially if a brace is rubbing or not fitting correctly. At the London Orthotic Consultancy, we have treated numerous international patients that have benefitted from specially designed braces that leave room to accommodate for growth and that can be adjusted remotely. Follow-up appointments for international patients are conducted via Skype.
This is a very common concern for patients considering treatment; in general, the dynamic chest compressor brace is easy to conceal if you are wearing a loose-fitting shirt for school or work. If you are wearing two chest braces – one for the main deformity and the other for rib flaring – then this may be more noticeable, especially under a t-shirt. Normally loose-fitting clothing will conceal the brace, though it’s likely it will be seen through tight-fitting clothes.
It is really important to continue exercising while going through bracing treatment. Exercise is fundamental to keeping the chest wall flexible. Our treatment programme incorporates a daily exercise routine of around 30-40 minutes of stretching using yoga poses, resistance bands, deep breathing exercises and general muscle stretches. Deep breathing exercises allow the lungs to expand against the chest wall, pushing it outwards.
Exercising with the brace on in the later stages of treatment can also make the chest correction more stable and permanent.
Swimming is one of the best forms of exercise to complement bracing treatment, as the body positions required to swim imitate the resistance band training designed to stretch the chest and increase its flexibility. Some swimming strokes are better for this than others, please check with your clinician. The brace should always be removed for contact sports and for swimming.
For most patients, one brace is often all that is needed to achieve a desired level of correction. They are each designed to last the duration of treatment and accommodate any growth that may occur in that time. Some patients have benefitted from having two braces – one to treat the main deformity and the other to treat rib flaring. For some pectus excavatum patients, having a brace apply pressure to the ribs – in addition to vacuum bell therapy – can greatly reduce the appearance of the depressed sternum area of the chest, forcing it upwards and outwards into a more corrective position.
If you are worried about your chest shape, or your child’s chest shape, then get in touch for a free Skype consultation with one of our pectus specialists who can assess their chest and discuss treatment options. We are always happy to communicate with local GPs, thoracic surgeons and consultants if a patient approaches us for bracing treatment after considering other options.

Join The London Orthotic Consultancy in celebrating Cerebral Palsy Awareness Day on March 25th. Learn just how important expert orthotic care is in enhancing mobility, independence, and quality of life for children and adults with cerebral palsy.

Introducing the Agilik™ smart orthosis, a cutting-edge, powered knee orthotic now available in the UK through the London Orthotic Consultancy. Unlike traditional KAFOs or heavy exoskeletons, the Agilik™ provides dynamic knee assistance and offers real-time support, reducing fatigue and improving posture. This pioneering, modern technology can help children and adults with lower limb weakness walk more efficiently and naturally. We are honoured to be selected as the exclusive paediatric specialist centre in the UK for the Agilik™ device.

When Sophie noticed her baby Max had a persistent flat spot on his head, she was told it would resolve naturally—but it didn’t. Seeking a second opinion led her to the London Orthotic Consultancy, where Max was diagnosed with severe plagiocephaly.

A little more than four years after the LOCband Lite's launch, we're proud to have successfully treated our 250th helmet therapy patient at our Romford clinic using our cutting-edge 3D-printed cranial band. After five months of treatment, her final scan showed that her asymmetry had decreased from 12 mm to 3 mm.

Sky News published an article this month quoting scientists at Southmead Hospital who claimed there was a lack of research into flat head syndrome and its treatment with cranial remoulding (helmet) therapy. This is our response.

With our non-surgical treatment plan, Alex achieved 100% chest correction in just two years. His treatment involved a combination of dynamic chest compressor and vacuum bell therapy treatment to address his pectus excavatum and rib flaring.

Learn how a custom carbon fibre AFO helped Gill regain mobility and comfort despite complex challenges from shin bone (tibia) removal. We created a truly tailored orthotic solution made from pre-preg carbon fibre at our Cambridge clinic.

Discover how bespoke orthotics and the OSKAR program with Elaine Owen transformed Archie’s life with cerebral palsy quadriplegia, helping him avoid a wheelchair and achieve greater mobility.